Frequently Asked Questions
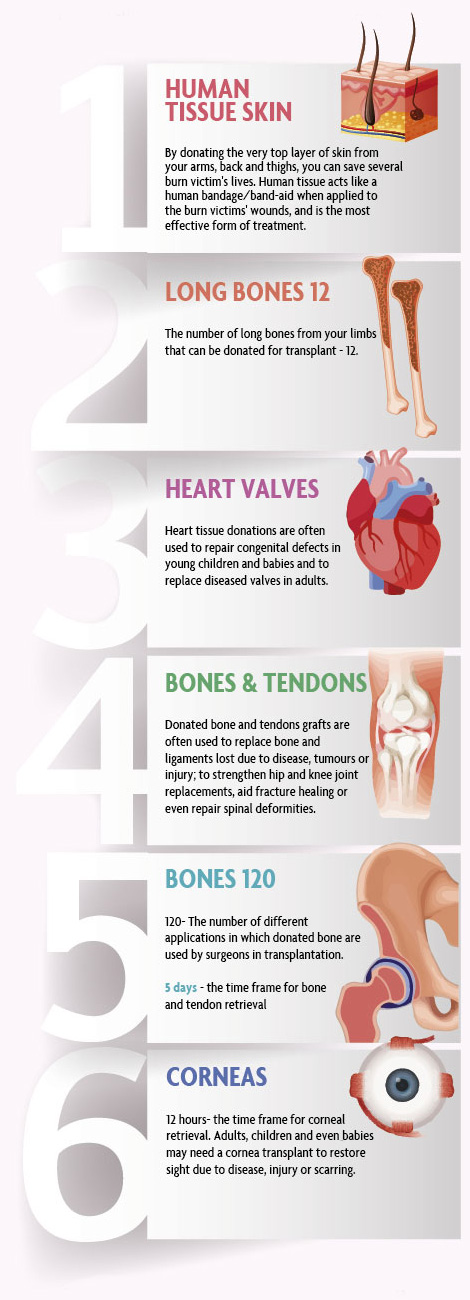
Which tissues are transplanted in South Africa?
Cornea, Bone, Tendons, Heart valves and Skin
Which organs are transplanted in South Africa?
Heart, Lungs, Liver, Kidney and Pancreas
Who can become a donor?
Any healthy individual between the ages of 15 and 80 years can donate tissue. A medical record that includes Cancer, Septicemia, Hepatitis and HIV Aids will exclude a potential donor.
Is tissue donation different to organ donation?
The concept is the same: A person decides that after his/her own death, another individual should benefit from healthy organs and tissue through transplantation – rather than these being committed to the grave.
How does this differ from organ donation?
Doctors will do their utmost to save a patient’s life, but in some case there is an irreversible loss of brain function, and the patient is declared clinically (and legally) dead.
About 1% of people die in circumstances in hospital that allow for successful organ donation. These circumstances seldom occur, however. To put this into context, statistics show that the greater population will either pass away at home, at work or on the road, under circumstances that prevent successful organ retrieval. In such cases the donor can donate tissue, which is equally as valuable and life-altering to a patient in need of a transplant. This means that a far greater number of people have the opportunity to donate tissue.
What is Bone and Tendon donation?
The long bones in the limbs (arms and legs) can be surgically removed and used for transplantation to patients who have suffered bone loss due to trauma, injury or disease and can provide renewed mobility and quality of life. The tissue is used in both Neuro and Orthopaedic procedures to improve quality of life in recipients.
Read more...
Musculoskeletal bone, tendons and cartilage are retrieved from the donor limbs (arms and legs) after death. Unlike organs, bone tissue can be donated several days after death and no tissue compatibility is necessary. Almost anyone can become a bone tissue donor and anyone a bone tissue recipient.
Bone is the second most commonly used donated tissue, second only to blood transfusions, and the need for bone tissue increases year on year.
Although not necessarily life-saving, bone implants can profoundly impact on the quality of life experienced by thousands of patients every year. Recipients’ normal, healthy, professional and active lives would not be possible without these essential transplants.
Currently more than 290 South African hospitals make use of bone allografts and medical specialists perform routine bone transplants in their fields of orthopaedic, reconstructive, dental, neurosurgical, and plastic surgery:
- Many patients suffer bone loss as a result of trauma or injury,joint replacement or arthritis.
- Some patients with tumours face possible amputation, but can behelped with allograft bone.
- In spinal fusion, allograft bone plays a very important role insupplementing and supporting the patient’s own bone.
- Treatment of some periodontal diseases affecting the jaw and gumsrequire bone tissue.
- Tendons are used to restore function to injured limbs.
Facts about bone tissue
Anyone between the age of 16 and 80 years can donate bone tissue, and no medical tests are necessary in order to become a bone tissue donor. There are certain factors that would render donor tissue unsuitable for transplantation, but each case is considered individually.
During the retrieval process, however, blood tests will be performed to screen for transmittable diseases like HIV and Hepatitis, thus guaranteeing the safety of the tissue to the recipient. The results of all medical tests are treated with utmost confidentiality.
What types of bone tissue are recovered?
- Bone is used for facial reconstruction, limb salvage, birth defect correction, (bone) cancer treatment, spinal and oral surgery. It is also used to replace bone destroyed by infection, tumours or trauma
- Cartilage is used for facial and other post-traumatic injury reconstructions
- Fascia (the fibrous tissue that covers muscles and tendons) are used in surgical repairs for sports injuries, craniotomy, ligament repairs, maxillofacial and other surgeries
- Tendons and ligaments are used to rebuild damaged joints
A bone graft transplant given to a patient who has developed bone cancer can mean the difference between limb amputation and saving the limb. Bone grafts can also assist fracture healing, strengthen bone surrounding hip and knee joint replacements, replace torn ligaments or repair spinal deformities.
Will the donor be treated with dignity?
The removal of bone tissue is no different from any other surgical operation, and is performed by highly skilled health professionals who adhere to the highest codes of conduct, ensuring that the donor’s body is always treated with dignity and respect. The donation of bone tissue does not alter the physical appearance of the donor’s body, and a prosthetic device is inserted in the area where tissue has been removed, to ensure that there is no disfigurement of the donor’s body. It is even possible for the donor’s family to view the donor’s body and if they so choose, to have an open casket funeral. It is also standard practice to retrieve tissue without compromising the funeral arrangements.
What is Cornea donation?
The thin, clear tissue layer in the eye that covers the iris and pupil is used in transplantation to give or restore sight to a blind or severely visually impaired person.
Read more...
What is a cornea?
The cornea is the eye’s outermost layer. It is the thin, transparent dome-shaped surface of the eye that covers the iris (coloured part of the eye), pupil and anterior chamber. Approximately the size of a one cent piece, the cornea forms the protective covering of the eye and focuses most of the incoming light.
Vision and the cornea – how does the cornea work?
Light first enters the eye, and is bent (refracted) by the cornea, it then becomes focused by the lens, before being projected onto the retina where the stimulation is interpreted by the brain as a visual picture or image.
The cornea acts as the eye’s outermost lens. Just as a camera lens focuses light onto film, the cornea focuses light onto a light-sensitive membrane called the retina. The retina functions much like the film inside the camera, and the iris like the camera shutter.
If the cornea becomes damaged or cloudy through disease, degeneration, infection or injury, the resultant scarring or discoloration causes impaired vision by blocking or distorting light as it enters the eye. Vision becomes dramatically reduced, and in some cases blindness may result. Severe damage of the cornea also impairs the protection of the eye from the drying environment and against infection.
What is a cornea transplant?
A cornea transplant is a micro-surgical procedure to remove all or part of a damaged (injured or diseased) cornea and replace it with healthy donor corneal tissue. A cornea transplant is often referred to as Keratoplasty or a corneal graft. It can be used to improve sight, relieve pain and treat severe infection or damage.
Who would need a cornea transplant?
Adults, children and even babies may need cornea transplants, for a variety of reasons. A transplant may be necessary in the case of cornea failure due to hereditary conditions such as Fuchs’ dystrophy, or Keratoconus (thinning and steep curving of the cornea). A transplant might also be required due to scarring resulting from trauma or injury, ulceration, infection or scarring as a result of previous ophthalmic surgery. Certain ageing processes can also affect the clarity and health of the cornea.
How great is the need for corneas and eye tissue?
Despite many hundreds of corneal graft surgeries taking place each year in South Africa, the need is ever increasing and unfortunately, never satisfied. To date, the use of artificial materials for corneal transplants has been unsuccessful. As a result, patients awaiting corneal transplants depend solely on the gift of tissue donation.
Should a donor elect to donate the complete eye, rather than the cornea alone, the sclera (white part of the eye) may be used in ocular graft procedures related to other types of eye disease.
Is there a time limit after death in which the corneas must be recovered?
Yes , the optimal recovery time limit after death is 12 hours, during which the Eye Bank personnel will need to procure the donated corneal or eye tissue.
How long does it take for the corneas or eye tissue to be procured and will this delay funeral arrangements?
The process of recovering the donated corneal or eye tissue and thereafter ensuring the preservation of the donor’s appearance takes approximately 30 minutes. Arrangements for this tissue recovery do not compromise funeral arrangements and the Eye Bank staff will usually liaise with the funeral home or hospital in this regard.
How soon will the donated corneas be used for transplantation?
A corneal transplant is usually performed 10 days of donation. This is dependent upon the completion of routine testing, the location of the receiving hospital, and the preparation of the selected recipient.
What is the procedure following corneal and scleratissue recovery?
Donated tissue is procured by trained personnel from the Eye Bank. Thereafter, the corneal or eye tissue is carefully stored in preservation media and transported to the Eye Bank where it is placed in a sterile environment within a temperature regulated medical grade walk-in refrigerator. After routine medical grade evaluations to identify infections or imperfections the donated corneal and eye tissue is made available for recipient selection and allocation. The donated tissue is then transported to the requesting recipient hospital in a controlled environment and using tracking procedures to ensure it is safely delivered.
This entire process entails the use of sterile, disposable consumables, professionally trained personnel and the facilities necessary to support resources for the efficient operation of the service. The fee levied covers associated procurement costs and ensures the continued development of the Eye Bank, an essential and community-driven healthcare resource within the Province. Patient recipients of grafts and transplants within State Hospitals receive corneal and eye tissue at the State Hospital’s expense. Private Medical recipients receive corneal and eye tissue which is usually reimbursed by their Medical Scheme.
Will the corneal / eye tissue recipients be informed of the identity oftheir donor?
No. The gift of sight is usually made anonymously. Specific information pertaining to the donor or donor family is not freely available to the recipient. However, the Eye Bank encourages recipients to write a letter of thanks to the donor family, which will then be forwarded on by the personnel. The Human Tissue Act does, however, make mention of an option for the two parties to meet, should both donor and recipient parties agree. In this case a written application must be submitted to the Eye Bank.
Who can qualify to become a cornea or eye tissue donor?
Any person between the ages of 6 and 65 years and even up to 70 years in certain cases, where death is as a result of either natural causes (for example heart diseases, most cancers, strokes) or unnatural circumstances (for example motor vehicle accident injuries, gunshot wounds, stab wounds). Cataracts and poor eyesight do not prevent eye donation, however, previous laser surgery to the eye and infections such as Tuberculosis and HIV Aids as well as Lymphoma and Leukemia are unfortunately contra-indications for donation. The Eye Bank personnel may be required to ask the next-of-kin, as well as the potential donor’s doctor for information on the health status and circumstances surrounding the death of the deceased, in order to determine whether the tissue may be suitable for donation.
Why become a cornea or eye tissue donor?
Sight is essential to the normal daily functioning and holistic life experience of an individual. Whether performing your occupation, caring for children or learning at school the gift of sight is enhanced through vision. Every year, more than 300 people in the Gauteng Province will have their sight preserved or restored through corneal transplantation. In addition to the cornea, the sclera (white part of the eye) can also be donated and used for ocular graft surgery in the treatment of cancer.
What is Heart Valve donation?
Sometimes, even when the heart is no longer beating, one’s heart can be donated and the aortic and pulmonary valves used to correct an abnormality in the heart of a patient, to not only improve but most probably save his or her life.
Read more...
What purpose would a donated heart valve serve?
Heart tissue donation enables the transplants of heart valves that improve or restore quality of lives, and can sometimes save the lives of people born with deformed hearts (genetic defects) or suffering from diseased or damaged valves.
Why the need for heart valves?
Heart tissue donations are often used to repair congenital defects in young children and babies and to replace diseased valves in adults.
Whilst artificial valves and even certain animal valves can also be used, human heart tissue is preferable because it is more resistant to infection, and can enable the recipient to lead a life without the need for ‘chronic’ blood thinning medication. This factor makes human heart valves safer for women of childbearing age and allows children to lead normal active lives.
Homografts, also known as human allograft heart valves, are increasingly used for heart valve repair.
The need for heart valves is alarmingly high and still on the increase: 2.5% of all adults in both poor and developing countries are in need of heart valves – either mechanical or biological. It is estimated that by 2020, as many as 250 million people worldwide will suffer from heart valve disease, of which some 150 million will require treatment in the form of heart valve transplants.
In South Africa, an average 24 per 1000 people suffer from rheumatic heart valve disease. Of these between 1,400 and 1,600 patients require heart valve surgery annually, but due to the critical shortage of donor heart tissue only around 350 recipients are fortunate enough to receive the surgery (this includes mechanical, animal and donor valves). By 2020 an estimated 1.37 million South Africans will require heart valves, of which some 400 to 500 will need homograft (human donor) valves.
In South Africa, where there are only ten specialist Heart Units equipped to perform this type of tissue transplant, an average of 55 patients will receive homograft valves annually. In a population of over 55 million people this percentage relates to less than 1 person per million.
It is also estimated that only 10 to 15% of paediatric patients in need of homograft valve replacements every year, will eventually receive this life saving procedure.
Apart from a severe donor heart tissue shortage, at least 40 to 50% of donated homograft valves are rendered unsuitable for transplantation due to various reasons (structural abnormalities, trauma, infections, leakage, etc.), which also drastically limits the availability of suitable valves for use in transplants.
What is Skin donation?
Only the very top layer of skin (epidermis) is carefully removed in some areas of the body and is used very effectively in the treatment and transplantation of burn victims.
Read more...
Skin donation introduction
The need for human skin for the treatment of burn victims is enormous.
Every year in South Africa, shack (informal housing) and bush fires result in an unacceptably high mortality rate, and oftentimes severe burn injuries. Known as thermal burns, these are the most common.
An estimated 12% of all unnatural deaths are attributable to burn wounds in South Africa, and tragically this is the most common external cause of death in children less than 4 years old. The global average for burn injury deaths numbers 5 in every 100 000 people, where our local mortality rate is 8.5 in 100 000.These deaths occur due to the severity of the burns, but more so because there are no effective, affordable synthetic treatment options available to patients.
In a country whose population exceeds 50 million people, statistics reveal that burn injuries account for an alarmingly high 3.2% of South Africans. Translated, this amounts to some 1.6 million people sustaining some degree of serious burn injuries annually. Of those, 0.2% will be classed as severe burn injuries – meaning that every month around 268 people (of which 161 are children) sustain major burn injuries and will require specialised treatment.
Skin donation
Skin grafts can save a life. Skin grafts are medically recognised as the most effective way to minimise scarring and promote healing of severe burns. Children in particular need skin grafts as a small burn or scald can cover most of their body. Often the severe burn injury patient will need to repeat the skin grafting process, until their burns heal sufficiently.
Why is donor skin needed to treat burn patients?
Skin has four essential bodily functions:
- retention of moisture and prevention of permeation
- regulation of body temperature
- protecting the body against harmful environmental effects and shieldingit from bacteria
- sensation
Think of your skin as a protective covering that shields your body from germs. It is filled with white blood cells that are designed to attack any invading harmful bacteria. In the event of severe burn injuries, this protective barrier is compromised, leaving the patient vulnerable to a multitude of risk factors, the worst of which are dehydration and infection.
The pain and trauma experienced by severely burned patients is excruciating and unbearable. Burn pain is one of the most intense and prolonged types of pain.
Burn wounds must be dressed to prevent dehydration and infection, but with the use of synthetic applications these dressings must be re-applied every 2 to 3 days. This means that each time a new dressing is applied, the patient is subjected to further trauma and pain, and several newly formed cells will be lost in the process. The result of this is that both the treatment process and the patient’s levels of discomfort are extended.
With the application of donor skin to the burn wounds, the patient’s body recognises the skin as human tissue and is subsequently ‘fooled’ into believing that it is the patient’s own and accepts it. This significantly reduces the agitation of the cells at the burn site, allowing the body to return to its’ primary functions of restoring and regeneration. Different to synthetic skin, the donor skin may be left on the wound for up to 2 weeks. During the 10 to 14 days the patient’s body is afforded an opportunity to heal itself, the donor skin providing protection against infection and dehydration.
After the two weeks, the donor skin has dried out, spontaneously and easily detaching from the wound, without causing further damage or pain. At this point the woundscan be assessed and re-application or further treatment options considered.
Although the donor skin is ultimately discarded, it provides a temporary lifesaving window which offers additional benefits to the patient:
- Reduction in hypermetabolic response
- Decreased infections
- Better wound bed preparation
- Increased survival rate
- Reduced hospital stay, quicker healing
- Reduced hypertrophic scarring
Through skin donation, one can not only help another person in need, but literally save the lives of others.
Is there a cost involved in donation?
No. There is no cost involved in the donation of any of the tissues to the donor’s family.
(Costs for the donation of tissues are covered by the relevant Tissue Bank. All other costs and arrangements for the funeral remain the responsibility of the donor’s family or estate).
Written consent is required for all tissue retrieval.
Is there a time limit after death in which the tissue must berecovered?
Yes , depending on the type of tissue – for example, the optimal recovery time limit after death for cornea is 12 hours, but in the case of bone tissue, the time limit is much longer and can still be recovered successfully up to 5 days after death.
Where is the tissue retrieval done?
A specially trained team conducts the procedure in either the hospital, the local mortuary or at the funeral home of your choice. Through the entire donation process the donor’s body is treated with utmost care and respect.
Will tissue transplant recipients pay for their donated tissue?
Yes. A standard nominal fee is levied for each of the respective tissues in order to cover costs associated with the recovery, procurement and processing of tissue.
Will the donor be treated with dignity?
The removal of (organs and) tissue is no different from any other surgical operation, and is performed by highly skilled health professionals who adhere to the highest codes of conduct, ensuring that the donor’s body is always treated with dignity and respect. The donation of (organs and) tissue does not alter the physical appearance of the donor’s body, and a prosthetic device is inserted in the place of the removed tissue to ensure that there is no cosmetic disfigurement of the donor’s body. It is even possible for the donor’s family to view the donor’s body and if they so choose, to even have an open casket funeral.
In the event of my loved ones' death who can I contact for urgentassistance?
Please contact one of our trained coordinators in your area to assist you:
You will be asked to provide the following details:
- Name of your loved one
- Cause of death
- Time of death
- Age of your loved one
- Is your loved one at a hospital or at a mortuary or undertaker?
- The city or town where your loved one is situated
- Your name, contact number and relation to the deceased
Alternatively, you may contact the Organ Donor Foundation on:
Toll Free Number: 0800 22 66 11
Emergency/After Hours: 082 318 4376
Website: www.odf.org.za
The Organ Donor Foundation representative will pass on the information provided to the nearest Transplant Centre or Tissue Bank.